This article was copublished with The 19th, a nonprofit newsroom covering gender, politics, and policy. Sign up for The 19th’s newsletter here.
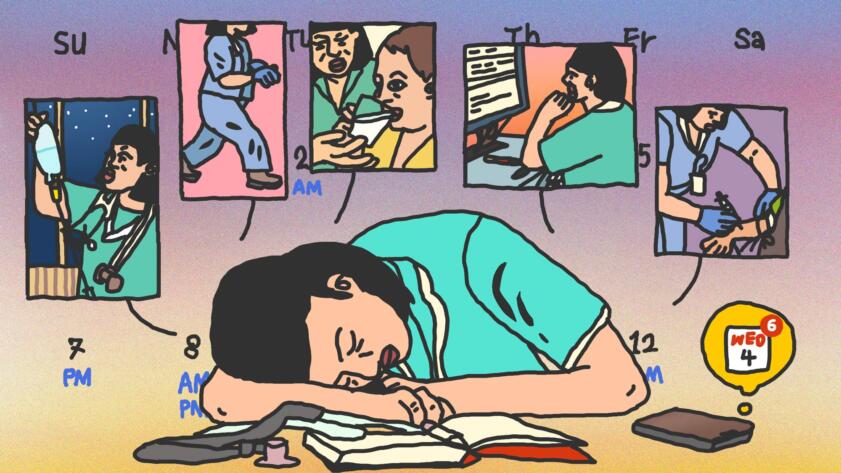
Shawnika Howell has been a nurse for 13 years, primarily in long-term care, but around the time of the winter 2021 COVID-19 surge, she decided to find some extra work through something new: an app called Clipboard.
The app lets nurses and nurse aides book individual shifts for a set number of hours with health care facilities, get paid, and move on to the next gig. Essentially, it’s Uber for nursing.
At first, Howell was attracted to the substantial and quick by-the-hour pay. Like other gig work apps, the rates health care facilities offer increase with demand. When she joined in 2021, gas prices were high, and nurses had been stepping away from their careers in droves, naming burnout and safety concerns as some of the reasons for leaving the profession. Apps like Clipboard offered nurses premium pay and the flexibility to choose the facilities they wanted to work for.
Howell wasn’t the only one interested.
Gig nursing apps have become hugely popular with both nurses and investors, as an estimated 100,000 nurses have left the profession since 2020 and demand for their labor remains high. Clipboard and ShiftKey—a similar nursing app—say tens of thousands of facilities now use their services. Clipboard has been valued at more than $1.3 billion by investors, and more recently, ShiftKey was valued at more than $2 billion.
But Howell eventually started to sour on Clipboard. The attendance policy runs on a points system. If a nurse fails to show for a shift, it deducts 85 of 100 points until workers earn them back through consistent attendance—over weeks or even months of shifts, depending on how often a person works. Once, when Howell was driving from Salinas, California, to a shift an hour away in San Jose, she missed a request from the app to confirm her attendance on the commute. By the time she showed up, another nurse had been assigned to the shift, and Howell was on the verge of temporary suspension from the app—she only had 15 points to spare. Eventually, she was restricted for a week after being late for a different shift.
She never knew what would happen until she showed up for a shift at a new facility, either. During a Clipboard shift at a long-term care facility, Howell said she was the only nurse working with about 40 patients, far more than usual. Mandated hours change based on the state and type of long-term care facility, but some experts have suggested patients receive around four hours of care per day.
You basically just hope that nothing goes wrong.
Shawnika Howell, nurse
Howell didn’t feel comfortable in the situation, she said, and tried to call Clipboard but couldn’t get through, so just did her best to get through the shift. “You basically just hope that nothing goes wrong,” she said.
Mostly, when issues came up, Howell found it difficult to push back or know where to bring her complaints. She couldn’t work out the attendance dispute that docked her 85 points, and after a problem with not getting paid for part of a shift, she spent a month emailing both the facility and Clipboard trying to sort it out.
“Nurses have all kinds of penalties that affect our attendance scores, and facilities should be required to respond regarding pay,” she said in an email to Clipboard in May trying to recoup her money. “Financially, this is inconvenient. It’s far too long.”
To better understand how turning nursing into a gig service affects patients, nurses, and health care facilities, The Markup filed public records requests and reviewed emails, facility inspection reports from federal regulators, complaints against Clipboard and ShiftKey, and subpoenas from a state department of labor. Together, this trove of documents depict what can go wrong in a center staffed by gig nurses, and how those nurses face limited recourse as their peers continue to leave the industry behind. A survey this year by the staffing company AMN Healthcare found 94 percent of nurses believed there was a moderate to severe shortage of nurses where they worked. The resulting burden overwhelmingly falls on one demographic: women, who make up about 87 percent of registered nurses, according to the Bureau of Labor Statistics.
With more traditional employment agreements, nurses might have a closer relationship with the facility and an easier time mediating problems, or a union to argue on their behalf. But like other industries where workers sign up for one-off gigs, nurses using Clipboard and ShiftKey are paid as contractors rather than as employees.
Short-term nurses, possibly from out of state and only there for a single shift, may be more ‘task-oriented’ than ‘care-oriented.’
Richard Mollot, Long Term Care Community Coalition
As a result of the one-off gig structure, nurses sometimes only work at a facility once, and care for patients they’ve never met before and won’t see again. This also means patients are sometimes receiving care from strangers, according to nurses who have used the apps, as well as inspection reports obtained by The Markup. Nurses also told us that they sometimes receive less training than they expect. The Markup found multiple reports in which facilities hiring nurses through ShiftKey and Clipboard did not provide training.
Richard Mollot, executive director of the advocacy group the Long Term Care Community Coalition, said in an interview that having the same caretaker over time instead of contracted nurses improves outcomes for patients.
“Over the years, it’s been very widely recognized that consistent assignment between a nursing team and residents is really important, both for the resident and the team itself,” he said. Short-term nurses, possibly from out of state and only there for a single shift, may be more “task-oriented” than “care-oriented,” he said.
Degrading the Bonds Between Patients and Nurses
Last year, at a nursing center providing short-term rehab and long-term care in Corpus Christi, Texas, a nurse aide assigned through ShiftKey was working with a resident with nervous system degeneration, muscle spasms, and weak bones, according to inspection reports of facilities by the Centers for Medicare & Medicaid Services (CMS) obtained by The Markup. The nurse aide was helping the resident use the toilet when she was distracted by another patient and left the room, leaving the patient alone, according to a health and safety review of the facility by federal investigators.

Pixel Hunt
“Out Of Control”: Dozens of Telehealth Startups Sent Sensitive Health Information to Big Tech Companies
An investigation by The Markup and STAT found 49 out of 50 telehealth websites sharing health data via Big Tech’s tracking tools
The resident’s emergency bathroom help light went on, and when the nursing aide returned, the resident was on the ground. She’d fractured her left leg, displaced her right, and had to be hospitalized. The inspection report questioned whether the aide had received proper training and determined the facility “did not provide the amount of supervision necessary” to prevent the fall. The aide told investigators she “was never educated by facility staff to stay with the resident at all times while toileting,” according to a summary of the conversation in the report.
“She stated, when you start working for the facility, the facility just tells her what hall she would be working but not how to look into how to care for the resident,” the report reads. Facility administrators told inspectors that they would no longer use the person from ShiftKey. No one at the company operating the Corpus Christi nursing center responded to requests for comment on the incident, including about whether the facility still hires through ShiftKey.
As technology makes gig work more common and accessible than ever, some critics worry that instant and one-off nursing shifts degrade the bonds between patients and health care workers, and make proper training of nurses more difficult.
“We’ve been struggling for decades to hold the health care industry accountable to staffing practices that serve our patients and our profession,” said Michelle Mahon, assistant director of nursing practice at the union National Nurses United. “We know that patients are safer and outcomes are better when there are more permanent staff.”
The problems that existed with temporary workers may be exacerbated even further with a “hyper-contingent” staff, she said. Effective training requires time that quick-turnaround gig work doesn’t incentivize, Mahon said.
In the short-term, nurses assigned to shifts also may not know where to find important equipment during an emergency, Mahon said. Nurses may also not be from the community where they’re working and feel less connected to their patients.
Getting it right is always really a matter of life and death in health care.
Michelle Mahon, National Nurses United
When a patient requires long-term care, nurses hired for brief periods may have less of an understanding of their routine and needs, Mahon said. If a nurse doesn’t understand a facility’s records system, they might fail to realize when a patient needs a specific type of medication. “Getting it right is always really a matter of life and death in health care,” she said. That type of training, she argues, can’t be given in a short training session.
A review of complaints conducted by The Markup shows multiple examples of gig nurses receiving incomplete training. In addition to the Corpus Christi case, federal inspectors reviewed a Louisiana facility’s staffing and training policies and found multiple deficiencies, including patients not receiving their prescriptions or receiving the wrong medication. According to the CMS report, an administrator told inspectors “no one at the facility was responsible for completing abuse/neglect training with agency staff, nor had anyone verified competency testing” before workers were allowed to work at the facility. The report said that over an eight-day period, there were 126 nursing shifts scheduled using workers from staffing agencies, and that none of those workers “had been verified for any training or competencies.” Instead, the administrator expected all agencies, including gig agencies like ShiftKey, to have performed the training. Inspectors noted that the 14 ShiftKey workers at the facility specifically did not have abuse and neglect training. It’s not clear from the reports how or whether those workers were involved in the incidents.
Regan Parker, general counsel and chief public affairs officer for ShiftKey, said in an emailed statement that the company’s role is “connecting facilities with fluctuating workforce needs directly with independent licensed professionals who have made the intentional choice to be independent, set their own schedule, establish their pay rate, and apply their skills while showing up for patients.” The company did not respond to questions about the inspection reports that found facility deficiencies in Texas and Louisiana, or about steps the company takes to ensure workers are properly trained.

Working for an Algorithm
When Drivers Are Attacked, Uber Leaves Police Waiting for Help
An investigation by The Markup found that Uber is slow to respond to law enforcement requests, leaving drivers vulnerable to repeated attacks
Gig Workers Have Fewer Protections—Nurses Are No Exception
Gig labor is a tension point in other areas of Big Tech, from ride-share drivers to food delivery. Nursing apps entered a market where worker classification has become a hot-button issue. Contractors have more flexibility and in some circumstances higher pay, but generally, workers classified as employees have rights to sick leave, minimum wage pay, and other benefits that contractors aren’t automatically granted.
Around the country, state legislation is being drafted to determine how and when workers are classified as employees or contractors. Nationally, the Biden administration has been pressing a proposed rule that would give gig workers more access to labor protections employees have, such as insurance and unemployment benefits. If enacted, Biden’s proposal would roll back the Trump-era framework that made it easier to classify gig workers as independent contractors.
In court, Uber and Lyft, in particular, have successfully defended their position that drivers are contractors, and throughout the legal dispute, Uber’s CEO said it couldn’t afford to hire its 50,000 drivers as employees overnight. But the companies making gig nursing apps wouldn’t necessarily collapse if they classified nurses differently: Other similar apps, like ShiftMed, already classify their workers as employees.
“Essentially, with a 1099 [tax form], you’re really supposed to be running your own business, which is not something that most nurses working as a 1099 would say that they’re doing,” said Dane Steffenson, a former U.S. Department of Labor attorney who now works in private practice at his own firm.
Steffenson says gig nurses are in a unique position compared to other workers, requiring highly specialized training for a lifesaving environment. “It’s very different if you’re walking into a long-term care facility or a hospital,” compared to being an Uber driver, he said.
The Labor Department has shown interest in cracking down on health care facilities when gig nurses aren’t paid what they’re owed. This year, the department publicly announced action against several staffing agencies that it said failed to pay nurses for overtime. In California, one lawsuit against a gig nursing app, Care.Stat!, alleged that workers were misclassified as contractors. The company denied the allegations but recently reached a settlement, according to court records.
When a dispute does come up, companies that classify their workers as contractors may have more room to distance themselves from the complaint than other companies assigning shift workers. Last year, for example, the Illinois Department of Labor asked Clipboard for more information on its business after multiple complaints over wages, according to emails between Illinois regulators and Clipboard that were obtained by The Markup.
The Illinois Nurse Agency Licensing Act regulates how nursing agencies operate, including deeming them “employees of the nurse agency.” But in a letter to regulators, Clipboard’s attorneys argued the law didn’t apply and that the company was only an online marketplace connecting nurses with facilities for a fee—not a staffing agency.
Sarah Bauer, a Clipboard Health spokesperson, said in a statement that workers who use Clipboard are required to affirm their status as independent contractors, and agree to the company’s attendance policy. Workers are encouraged to report any safety concerns, Bauer said. Bauer did not directly address the criticism that shift work degrades bonds between patients. In response to a question about Howell’s experience, Bauer cited the company’s attendance policy, and said the company encourages workers to report safety concerns.
MarketWatch recently reported on a California nurse aide who claimed she was owed $21,000 in unpaid work from Clipboard, eventually losing her home while she tried to get the funds. Clipboard did not respond to MarketWatch’s questions about this specific nurse.
That nurse and others might have been able to turn to organized labor for help, but as contractors, workers don’t have the same ability to form a union for protection. For unions like National Nurses United, the potential shift in classification is an almost existential threat.
“This push to this model allows them to compartmentalize the work, so nurses don’t have relationships with each other, so they can’t organize and demand safe staffing conditions,” along with other protections workers have fought to gain over decades, Mahon said. Classifying nurses as contractors, then, ultimately gives companies more power over workers, and limits workers’ ability to hold them accountable, she believes.
“They really just wash their hands of all of their obligations,” she said.